Postpartum hemorrhage (PPH) – defined as a blood loss of 500 ml or more within 24 hours of birth – affects one in every six women giving birth. PPH continues to be the leading global cause of maternal mortality, with deaths occurring overwhelmingly in low- and middle-income (LMIC) settings. Some medicines for the prevention and treatment of PPH have been well-known for decades (i.e., oxytocin, ergometrine, and misoprostol) while others are more recent additions.
In 2018, WHO updated its PPH treatment recommendations to include the administration of tranexamic acid (TXA) via intravenous route within 3 hours of birth in women with PPH (regardless of the underlying cause of PPH). Also, in 2018, WHO updated its PPH prevention guidelines to include the use of heat-stable carbetocin (HSC) and to provide expanded guidance on the selection of uterotonics for PPH prevention. Some of the uterotonic medicines (oxytocin and misoprostol) have other obstetric uses, such as induction and augmentation of labor. In contrast, others are actually contraindicated for these uses and may cause harm if misused.
For a summary of information on the suite of PPH products that can be used for the prevention and treatment of post-partum hemorrhage and other obstetric uses.
Key International Guidelines, Statements and Resources
- WHO/UNFPA/UNICEF Joint Statement on Appropriate Storage and Management of Oxytocin – A Key Commodity for Maternal Health (2019)
- WHO/UNICEF Joint Statement on Temperature-Sensitive Health Products in the Expanded Programme on Immunization Cold Chain
- PPH Roadmap
- WHO recommendations: Uterotonics for the prevention of postpartum heamorrhage (2018)
- WHO recommendations for the prevention and treatment of postpartum haemorrhage
- Regulatory guidance for assessment and management of applications for marketing authorization of oxytocin
- Oxytocin quality: Evidence to support updated global recommendations on oxytocin for postpartum hemorrhage
WHO/UNFPA/UNICEF Recommend 'Three Urgent Actions'
Building upon the work of the United Nations Commission on Life-Saving Commodities for Women and Children, WHO, UNICEF and UNFPA issued a statement that recommends three actions to ensure effective management of and access to quality oxytocin.
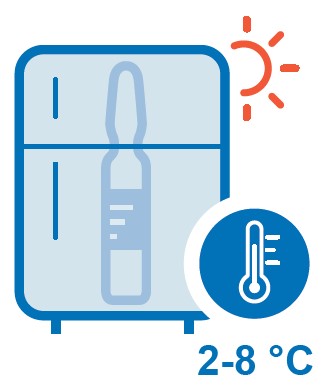 1. Supply chain managers should ensure that oxytocin is maintained at 2-8 ℃ (36-46 ℉).
1. Supply chain managers should ensure that oxytocin is maintained at 2-8 ℃ (36-46 ℉). 2. Procurers and distributors of oxytocin should ensure that specifications clearly reference appropriate quality standards and requirements, including appropriate labelling for storage at 2-8 ℃ (36-46 ℉).
2. Procurers and distributors of oxytocin should ensure that specifications clearly reference appropriate quality standards and requirements, including appropriate labelling for storage at 2-8 ℃ (36-46 ℉).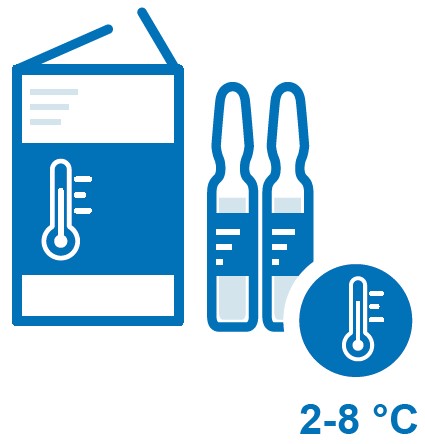 3. Medicine regulators should support and enforce labelling and marketing to reflect appropriate cold chain maintenance at 2-8 ℃ (36-46 ℉).
3. Medicine regulators should support and enforce labelling and marketing to reflect appropriate cold chain maintenance at 2-8 ℃ (36-46 ℉).The Approach
The USAID Global Health Supply Chain Program-Procurement and Supply Management (GHSC-PSM) project leads efforts to improve PPH product quality in LMICs. GHSC-PSM synthesizes the most up-to-date evidence on oxytocin quality and develop new approaches to ensure its quality throughout the supply chain. The project collaborates with global partners—such as WHO, UNICEF and UNFPA—to develop guidance on appropriate storage and management of PPH products and support implementation of the guidance in select countries.
Using a holistic approach, we support national governments in their efforts to strengthen procurement and supply management practices to ensure PPH product quality in the following areas:
- Regulatory environment. Oxytocin degrades when it is exposed to high temperatures, and product labelling may confuse supply chain managers and health care providers. GHSC-PSM supports regulatory efforts to ensure that oxytocin is labelled for storage between 2-8° C.
- Policy and finance. National level policy and financing strategies often affect the availability of quality PPH products. In our approach, GHSC-PSM considers how policy and financing strategies impact procurement and supply management of PPH products. Understanding how oxytocin is purchased—whether through donor resources, national budgeting and allocation processes, or insurance schemes—informs strategies that improve the availability of affordable, quality uterotonics and TXA.
- Procurement and sourcing practices. Procurement agents at all levels of the health system need to source and procure quality products. Oxytocin must have appropriate storage conditions on the label and misoprostol Tablets must be packed in Alu/Alu blisters with appropriate storage conditions on the label. GHSC-PSM considers how different procurement mechanisms can streamline and improve oxytocin procurement practices.
- Forecasting and supply planning processes. Accurate forecasting and supply planning help ensure consistent availability. Deficiencies in this area can lead to stockouts and may prompt health care and supply chain staff to buy medicines from the unregulated sources. To this end, GHSC-PSM provides forecasting and supply planning technical assistance to ensure that the right quantities of quality products reach women when and where it is needed.
- Logistics and inventory management systems and infrastructure. Due to oxytocin’s heat sensitivity, WHO recommends that oxytocin be stored between 2-8° C. In many LMICs, cold chain storage infrastructure may be weak or insufficient. GHSC-PSM develops strategies — such as integrating oxytocin into the Expanded Programme on Immunization cold chain or increasing the frequency of ordering—to that oxytocin is stored appropriately.
Implementation Resources
Advocacy
- Buy Quality Oxytocin, Keep It Cold: An Advocacy Messaging Framework for Oxytocin, the First-Line Drug for the Prevention and Treatment of Post-Partum Hemorrhage (English, French, Spanish)
- Oxytocin – Evidence for Action: an analysis of the evidence that low and middle‑income governments need to prioritize decisive action to improve access to quality uterotonics to reduce preventable PPH (English)
- Medicines We Can Trust
- Bleeding after Birth Complete 2.0 Preventing deaths from postpartum hemorrhage
Stability Testing and Product Labelling

Procurement
Storage and Distribution
Quality of Oxytocin in LMICs: Results from Postmarketing Surveillance Studies
Location | Title | Author, Year | Selected Results |
Democratic Republic of the Congo | Lambert et al., 2018 | 80% out specification | |
Nigeria | Anyakora et al., 2018 | 74.2% out of specification | |
Nepal, Vietnam | The degradation of pharmaceutical oxytocin samples in Nepal and Vietnam | M. Lui et al., 2016 | 31% out of specification |
15 countries | Torloni et al., 2016 | 45.6 % median prevalence of oxytocin samples did not pass quality testing as defined by authors; 36.0% out of specification | |
Burkina Faso, Kenya, Madagascar, Nepal, Nigeria, Tajikistan, Tanzania, Vietnam, Zimbabwe | World Health Organization, 2015 | 64% out of specification | |
India | Stanton et al., 2014 | 36.2% out of specification | |
Ghana | Ghana Food and Drugs Authority (FDA) Laboratory Services Department, 2013 | Assay: 55.6% out of specification (2% of these had 0% API); 10% failed assay but passed sterility
Sterility: 40% of samples failed sterility but passed assay; 45% of samples failed both assay and sterility tests 97.5% of samples failed sterility, assay, or both | |
Ghana | Stanton et al., 2012 | 73.9% out of specification; 4.3% expired | |
Zimbabwe | Hogerzeil et al., 1993 | 1 of 6 samples expired; of remaining 5 samples, 80% out of specification | |
WHO Drug Information 2016; 30(1) |




